Epidural And Combined Spinal Epidural Anatomy Indications And
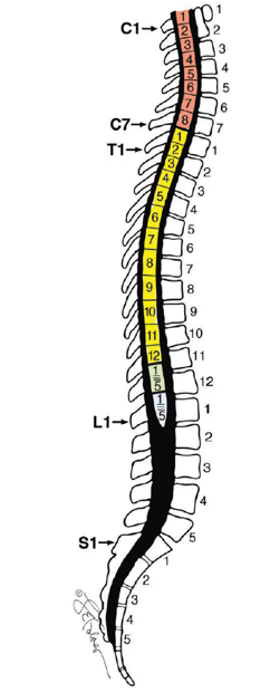
Epidural And Combined Spinal Epidural Anatomy Indications And Anatomy the vertebral column consists of 33 bones, including 7 cervical, 12 thoracic, 5 lumbar, 5 fused sacral, and 3 to 5 (most commonly 4) fused coccygeal vertebrae. 1 3 spinal anesthetics target the lumbar and caudal regions, whereas epidurals have a wider range of applicability and include the thoracic space. Spinal, epidural, and combined spinal epidural (cse) anesthesia can be used for many of the same surgical procedures. differences among them may affect the choice of technique for a specific procedure or patient. the advantages and disadvantages of the various neuraxial anesthesia techniques are shown in a table . spinal anesthesia is usually.
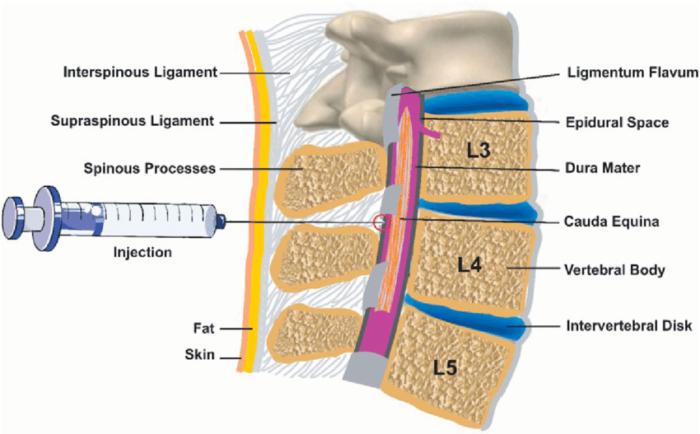
Epidural And Combined Spinal Epidural Pharmacology Technique And Introduction. neuraxial analgesia is the most effective and most commonly used therapy for pain relief during labor and delivery. epidural, combined spinal epidural (cse), and other central neuraxial techniques, including dural puncture epidural (dpe), single shot spinal, and continuous spinal analgesia, are among the many options available to alleviate the pain of childbirth. In this video, i show how to place an epidural, spinal, and combined spinal epidural while explaining the differences between these neuraxial blocks. warning. Combined spinal epidural anesthesia plays a valuable role in the armamentarium of anesthesiologists by offering many of the advantages of spinal and epidural anesthesia while minimizing the risks associated with each technique. 3 proper use of this technique requires an intimate understanding of the interrelationship of the epidural space, its contents, and the thecal sac. additionally, one. Needle through needle—first described in 1982, this most commonly used technique involves locating the epidural space with a needle and subsequently inserting a small diameter spinal needle through the epidural needle lumen to administer local anesthetic intrathecally. once the spinal needle is removed, the epidural catheter may be inserted into the lumen of the epidural needle and placed in.
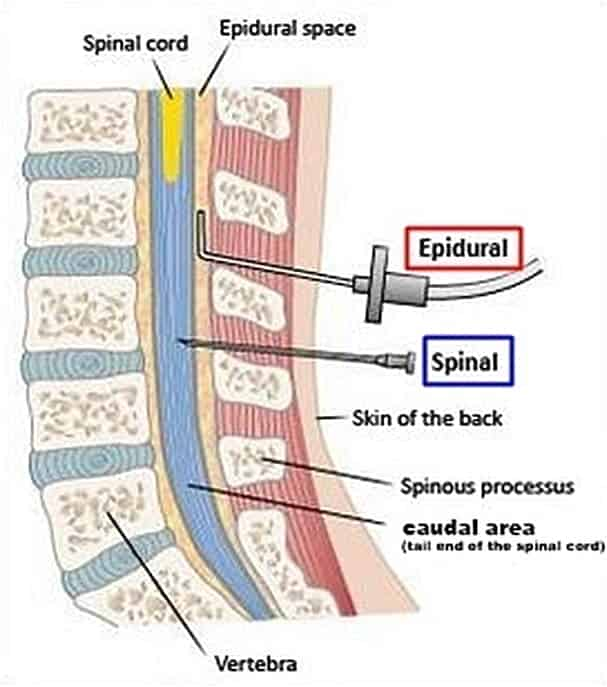
Spinal Epidural Bonesmartв Combined spinal epidural anesthesia plays a valuable role in the armamentarium of anesthesiologists by offering many of the advantages of spinal and epidural anesthesia while minimizing the risks associated with each technique. 3 proper use of this technique requires an intimate understanding of the interrelationship of the epidural space, its contents, and the thecal sac. additionally, one. Needle through needle—first described in 1982, this most commonly used technique involves locating the epidural space with a needle and subsequently inserting a small diameter spinal needle through the epidural needle lumen to administer local anesthetic intrathecally. once the spinal needle is removed, the epidural catheter may be inserted into the lumen of the epidural needle and placed in. Epidural anesthesia is a method of neuraxial pain control in which anesthetic medications are injected into the epidural space to block sensory and motor spinal nerve roots in the thoracic, abdominal, pelvic, and lower extremity areas. this epidural technique can be used for anesthesia during procedures, chronic pain, or muscle spasticity as a primary anesthetic or pain management adjuvant. Having low blood pressure, which can make you feel lightheaded. experiencing a severe headache caused by spinal fluid leakage. less than 1% of people experience this side effect. getting an infection from the epidural procedure, such as an epidural abscess, discitis, osteomyelitis or meningitis.

Comments are closed.